Effective medications today can cure hepatitis C virus (HCV) infection in only a few months and prevent liver cancer and severe liver damage from chronic infection. However, most patients in safety-net primary care practices are not being screened for the virus. This includes baby boomers, the post-World War II generation most at risk for chronic HCV infection and progression to liver cancer.
Testing a new intervention to address this issue, a team from the Long School of Medicine at The University of Texas Health Science Center at San Antonio targeted five federally qualified health centers and one family medicine residency program that serve low-income communities with largely Hispanic populations. A grant from the Cancer Prevention and Research Institute of Texas (CPRIT) and a Section 1115 Medicaid waiver from the Centers for Medicare and Medicaid Services supported the research program.
“Our program, ‘Screen, Treat or Prevent Hepatocellular Carcinoma and Hepatitis C Virus (STOP HCC-HCV),’ aims to arrest the rise in Texas liver cancer by building the capacity of primary care settings to screen for HCV infection as well as to manage and treat infected patients within their medical home through teleconsultation,” said study co-author Andrea Rochat of the Long School of Medicine. Rochat is a senior research coordinator with the university’s Center for Research to Advance Community Health (ReACH).
A multi-component strategy utilized in the six safety-net practices increased baby boomer screening rates for HCV infection from less than 1% to 48%. Across the six practices, 13,334 of 27,700 baby boomers were screened. Results were published in December in the journal Annals of Internal Medicine.
Small practices that manage uninsured patients lack the infrastructure necessary to accomplish widespread HCV screening, the researchers found. Nationally, screening rates are less than 20%. “In the practices we studied, HCV screening of baby boomers was not happening at baseline,” said study senior author Barbara J. Turner, M.D., who led the study at the Long School of Medicine and is transitioning to the University of Southern California’s Keck School of Medicine. “After implementation of our strategy, screening rates ranged from 19% to 70% across diverse safety-net practices serving primarily underinsured, Hispanic populations.”
“South Texas is disproportionately affected by liver cancer,” said study co-author Sarah Lill of the ReACH Center. “HCV infection can be cured to significantly reduce the risk of liver cancer that affects predominantly low-income populations like the one in our study.”
Task force guidelines
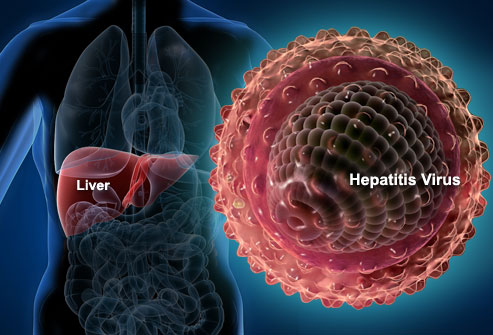
HCV infection is underdiagnosed and can persist in a patient for decades before presenting symptoms. The U.S. Preventive Services Task Force in 2013 recommended one-time HCV screening for all persons born in 1945 through 1965 (baby boomers). Three-fourths of people infected with HCV are in that age group and were infected years ago due to less-effective sterilization in health care delivery, injection drug use and blood transfusions before HCV screening.
“It is estimated that 1.5 million people in the U.S. have chronic HCV infection and don’t know it,” said co-author Raudel Bobadilla of the ReACH Center. “It’s a huge public health issue.”
Since 2013, the prevalence of HCV has increased in younger persons, and oral direct-acting antiviral medications have been introduced to treat the disease safely and quickly. These medicines cure HCV infection in a large majority of patients.
The Preventive Services Task Force in August 2019 released a draft recommendation statement seeking public input on expanding one-time screening for HCV infection to all adults ages 18-79. “Although these guidelines are still considered to be a draft, the field recognizes that these will likely become formal guidelines soon,” Lill said. “When our program started, national guidance was to screen baby boomers.”
“This screening guideline definitely requires an effective infrastructure within primary care – not just for screening but also for treatment and long-term management,” Rochat said. “The infrastructure that we refined through the STOP HCC-HCV program can inform future models for all-adult HCV screening.”
Casting a wide net
STOP HCC also developed training programs and teleconsultation specialist support so that primary care physicians could treat their uninsured patients with chronic HCV infection. These patients cannot access specialist care but are able to receive effective medications to cure HCV through programs for low-income persons. The project has been able to cure 95% of the uninsured patients who started treatment through STOP HCC.
Funding for the project was partly through CPRIT, the state agency funded by an initial $3 billion authorized by Texas voters in 2007 and reinfused with another $3 billion by voters in November 2019. “Texas is unique to have CPRIT to fund implementation science that tries to improve screening and management of liver disease in low-income patients; most states don’t have anything like it,” said Ruben Mesa, M.D., director of the Mays Cancer Center, home to UT Health San Antonio MD Anderson Cancer Center.
According to the American Cancer Society, 4,300 Texans were diagnosed with liver cancer in 2019 and 2,800 died of the disease. Worldwide, long-term infection with hepatitis C and hepatitis B virus is the most common risk factor for liver cancer.
Safety-net primary care practices’ low rates of HCV preventive screening are in stark contrast to the U.S. Department of Veterans Affairs’ excellent program. The VA screens 75% of baby boomers for HCV.
“The VA has been very successful with its program because all of its patients are insured and can access testing and treatment,” Dr. Turner said. “These are obstacles in the smaller primary care practices that serve low-income populations.”
Summarizing the funding, she said, “The take-home message is that we have national guidelines to test every baby boomer and may shortly have recommendations to test all adults for HCV, but we need to develop and support the infrastructure to put screening and management into place for vulnerable populations.”
# # #
The Long School of Medicine at The University of Texas Health Science Center at San Antonio is named for Texas philanthropists Joe R. and Teresa Lozano Long. The school is the largest educator of physicians in South Texas, many of whom remain in San Antonio and the region to practice medicine. The school teaches more than 900 students and trains 800 residents each year. As a beacon of multicultural sensitivity, the school annually exceeds the national medical school average of Hispanic students enrolled. The school’s clinical practice is the largest multidisciplinary medical group in South Texas with 850 physicians in more than 100 specialties. The school has a highly productive research enterprise where world leaders in Alzheimer’s disease, diabetes, cancer, aging, heart disease, kidney disease and many other fields are translating molecular discoveries into new therapies. The Long School of Medicine is home to a National Cancer Institute-designated cancer center known for prolific clinical trials and drug development programs, as well as a world-renowned center for aging and related diseases.
The University of Texas Health Science Center at San Antonio, dba UT Health San Antonio, is one of the country’s leading health sciences universities and is designated as a Hispanic-Serving Institution by the U.S. Department of Education. With missions of teaching, research, healing and community engagement, its schools of medicine, nursing, dentistry, health professions and graduate biomedical sciences have graduated more than 37,000 alumni who are leading change, advancing their fields and renewing hope for patients and their families throughout South Texas and the world. To learn about the many ways “We make lives better®,” visit www.uthscsa.edu.
Stay connected with The University of Texas Health Science Center at San Antonio on Facebook, Twitter, LinkedIn, Instagram and YouTube.