Scientists developing medication to help substance users for weeks
Naloxone (brand name Narcan®) currently is used to rescue people from opioid overdose, but the protection is transient, lasting an hour or less. Opioid effects can persist for several hours, however, which puts the individual at risk of overdose re-emerging as effects of naloxone wear off.
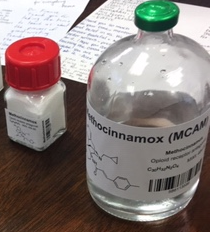
Researchers in the Long School of Medicine at The University of Texas Health Science Center at San Antonio and with the University of Bath, U.K., are developing a long-lasting anti-opioid drug – called MCAM – to address this problem. Their vision is to administer a single injection of MCAM and protect against opioid overdose not just for hours, but for weeks or longer.
“This drug would have tremendous application for people who have a high risk of overdose,” said project leader Charles P. France, Ph.D., professor of pharmacology and psychiatry who occupies the Robert A. Welch Distinguished University Chair in the Long School of Medicine.
In published research, a single administration of MCAM blocked the effects of heroin and fentanyl in rodents and nonhuman primates for several weeks, Dr. France said.
MCAM, short for methocinnamox, was discovered by University of Bath professors John W. Lewis, Ph.D., and Stephen M. Husbands, Ph.D., who continues to perform medicinal chemistry to optimize its properties. MCAM blocks the places in the brain where opioid drugs such as heroin and fentanyl attach and produce their effects. Naloxone does this, too, but MCAM attaches much tighter, accounting for its very long duration of action and the inability of opioids to overcome blockade by MCAM, Dr. France said.
‘We are losing 70,000 people per year’
Naloxone is the only drug currently available to treat opioid overdose. Three other drugs, buprenorphine, methadone and naltrexone, are approved to treat opioid use disorder, which is a clinically defined pattern of opioid abuse. Buprenorphine and methadone are heroin-like drugs that can produce a high, are diverted and abused, and interact with other drugs in a manner that can increase the risk of overdose. A safe alternative to them would be welcomed. Naltrexone, meanwhile, acts like naloxone and has a duration of action that is somewhat longer than naloxone, but this activity is not long enough to provide sustained protection from the effects of opioids.
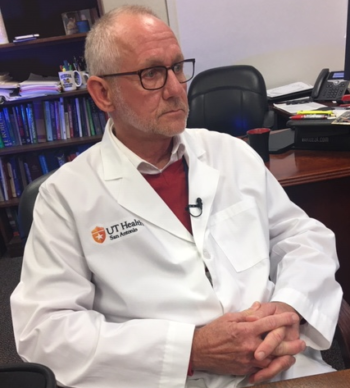
“These drugs have been around for decades, yet we are still losing 70,000 people per year to opioid overdose,” Dr. France said.
In addition to rescuing from overdose, MCAM could be used to treat opioid use disorder because it blocks the euphoria that contributes to abuse of opioids. Long-lasting relief from opioid addiction would be tremendously important, particularly in regions where physicians and especially addiction psychiatrists are in scarce supply.
“Much of the opioid crisis in the United States is occurring in rural America, where there is less access to health care,” Dr. France said. “You can imagine that being able to give a single injection of MCAM and protect someone from the addictive properties and adverse effects of opioids for months or longer could change many lives for the better.”
‘We have to get this right’
Twenty people in laboratories at the Long School of Medicine are working on MCAM. “We recently received two grants from the National Institute on Drug Abuse, one of the National Institutes of Health, to investigate the basic science of this drug and work out the details in cells and animals,” Dr. France said. “We recently received another grant that will eventually help us get U.S. Food and Drug Administration approval to bring MCAM into phase I (first-in-human) clinical trials.”
The timeline to possible human trials is two years, Dr. France said.
“We have to get this right. There is an urgency,” he said.
# # #
Acknowledgments:
Collaborators from the Long School of Medicine at The University of Texas Health Science Center at San Antonio include Kelly A. Berg, Ph.D.; William P. Clarke, Ph.D.; Lisa R. Gerak, Ph.D.; Martin Javors, Ph.D.; David R. Maguire, Ph.D.; and James H. Woods, Ph.D. Dr. Woods and Dr. France are co-owners of a U.S. provisional patent on all uses of MCAM for substance use disorders. Dr. Woods previously studied MCAM at the University of Michigan. The research team collaborates with Stephen M. Husbands, Ph.D., of the University of Bath, U.K. Dr. Husbands and Dr. Woods published the first journal article on the MCAM molecule.
References:
“Methocinnamox is a Potent, Long-Lasting, and Selective Antagonist of Morphine-Mediated Antinociception in the Mouse: Comparison with Clocinnamox, β-Funaltrexamine, and β-Chlornaltrexamine,” Journal of Pharmacology and Experimental Therapeutics, Jillian H. Broadbear, et al., 2000 (the first publication on MCAM)
“Methocinnamox Produces Long-Lasting Antagonism of the Behavioral Effects of µ-Opioid Receptor Agonists but Not Prolonged Precipitated Withdrawal in Rats,” Journal of Pharmacology and Experimental Therapeutics, Lisa R. Gerak, et al., 2019
“Reversal and Prevention of the Respiratory-Depressant Effects of Heroin by the Novel μ-Opioid Receptor Antagonist Methocinnamox in Rhesus Monkeys,” Journal of Pharmacology and Experimental Therapeutics, Lisa R. Gerak, et al., 2019
“Long-Lasting Effects of Methocinnamox on Opioid Self-Administration in Rhesus Monkeys,” Journal of Pharmacology and Experimental Therapeutics, David R. Maguire, et al., 2019
Funding:
National Institute on Drug Abuse of the National Institutes of Health (USA) and the Welch Foundation.
# # #
The Long School of Medicine at The University of Texas Health Science Center at San Antonio is named for Texas philanthropists Joe R. and Teresa Lozano Long. The school is the largest educator of physicians in South Texas, many of whom remain in San Antonio and the region to practice medicine. The school teaches more than 900 students and trains 800 residents each year. As a beacon of multicultural sensitivity, the school annually exceeds the national medical school average of Hispanic students enrolled. The school’s clinical practice is the largest multidisciplinary medical group in South Texas with 850 physicians in more than 100 specialties. The school has a highly productive research enterprise where world leaders in Alzheimer’s disease, diabetes, cancer, aging, heart disease, kidney disease and many other fields are translating molecular discoveries into new therapies. The Long School of Medicine is home to a National Cancer Institute-designated cancer center known for prolific clinical trials and drug development programs, as well as a world-renowned center for aging and related diseases.
The University of Texas Health Science Center at San Antonio, also referred to as UT Health San Antonio, is one of the country’s leading health sciences universities and is designated as a Hispanic-Serving Institution by the U.S. Department of Education. With missions of teaching, research, patient care and community engagement, its schools of medicine, nursing, dentistry, health professions and graduate biomedical sciences have graduated more than 37,000 alumni who are leading change, advancing their fields, and renewing hope for patients and their families throughout South Texas and the world. To learn about the many ways “We make lives better®,” visit http://www.uthscsa.edu.
Stay connected with The University of Texas Health Science Center at San Antonio on Facebook, Twitter, LinkedIn, Instagram and YouTube.