Lower levels of a protective protein lead to liver inflammation, scarring
Contact: Will Sansom, 210-567-2579, sansom@uthscsa.edu
SAN ANTONIO (Oct. 3, 2023) — Researchers at The University of Texas Health Science Center at San Antonio (also called UT Health San Antonio) have identified a molecular pathway that connects aging to end-stage liver disease. A set of mechanistic processes, observed in mice fed an ethanol diet to mimic alcohol-related liver injury, offers clues for why older people suffer more serious and persistent liver damage than younger people do, even after liver injury is stopped.
The laboratory of Mengwei Zang, MD, PhD, at the health science center’s Sam and Ann Barshop Institute for Longevity and Aging Studies, reported the findings earlier this year in Aging Cell.
“Why are older individuals more likely to develop chronic liver disease compared to the young?” said Zang, professor of molecular medicine and the Ewing Halsell Distinguished Chair in Research at UT Health San Antonio. “What goes wrong with the aging liver that increases the risk of liver disease? Can we reverse these processes and maintain a younger, healthier liver? We seek answers to these questions.” Zang is also associate director of the South Texas Medical Scientist Training Program, which is the National Institutes of Health-funded MD-PhD dual-degree program at the health science center.
Liver fibrosis (or scarring) progresses in affected individuals during aging, and the cause was a mystery, Zang said. No approved treatment is available for this condition, even as the United Nations projects that the global population of people over the age of 65 will reach 1.5 billion by 2050. “A growing concern is the rising prevalence of complex chronic diseases, such as liver fibrosis, among older adults,” Zang said. “Tackling age-onset liver diseases is becoming an urgent public health and economic challenge.”
A team that included graduate students in UT Health San Antonio’s Personalized Molecular Medicine Program conducted the study. Students Jennifer Adjei-Mosi, Steven Blake Smithson and Gavyn Shealy, and a postdoctoral fellow in the lab, Qing Sun, MD, PhD, shed light on the link between SIRT1, a protein that promotes longevity but declines dramatically with aging, and NLRP3, a protein that regulates inflammation.

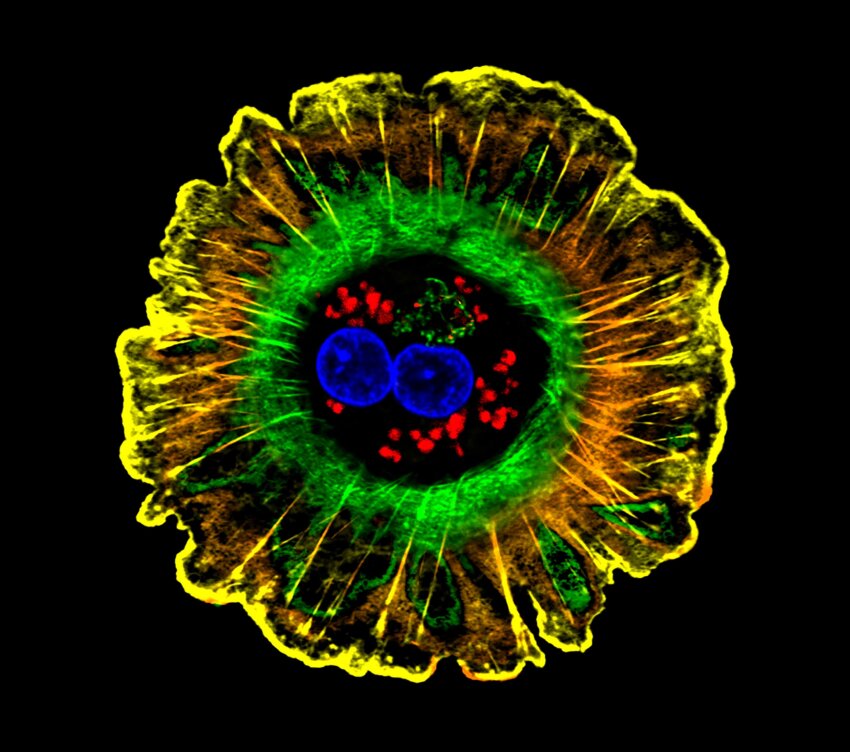
“Age-related loss of SIRT1 in the liver accelerated the progression of liver fibrosis by promoting NLRP3-mediated inflammation and by increasing hepatic stellate cells, a liver cell type responsible for producing collagen proteins that contribute to formation of scarring,” Zang said.
Young mice were observed to reverse liver fibrosis after injury cessation. Over time, hepatic stellate cell activation lowered, likely due to the restoration of hepatic SIRT1, which corralled NLRP3 activity.
In older mice, a severe form of liver fibrosis continued even after the injury ceased. “It was difficult to resolve the fibrosis that had developed,” Zang said. In these mice, as in older humans and animals, hepatic SIRT1 levels were very low.
Hepatic stellate cells are calm in the normal liver, but they secrete collagen when activated. The effect is a very stiff and thick scaffold of scar tissue called extracellular matrix. Collagen is one part of this matrix.
To test the hypothesis that diminished hepatic SIRT1 in old mice results in NLRP3-induced inflammation and scar formation, the Zang lab tested a known NLRP3 inhibitor called MCC950. In older mice given MCC950, alcohol-induced fibrosis resolved as NLRP3 signaling decreased, reducing inflammation, and stellate cell activation lessened, halting collagen deposition.
“Interventions such as NLRP3 inhibitors could help to keep the liver younger and healthier, reducing liver inflammation and slowing the progression of age-related liver fibrosis,” Zang said.
Most preclinical studies aimed at understanding liver fibrosis are performed in young mice, she said. Zang suggested that researchers could use older mice in developing drug therapies for liver fibrosis associated with aging, because her laboratory findings indicate that the ability of older livers to resolve liver fibrosis may be diminished compared to young livers.
Age-dependent loss of hepatic SIRT1 enhances NLRP3 inflammasome signaling and impairs capacity for liver fibrosis resolution
Jennifer Adjei-Mosi, Qing Sun, Steven Blake Smithson, Gavyn Lee Shealy, Krupa Dhruvitha Amerineni, Zerong Liang, Hanqing Chen, Mei Wang, Qinggong Ping, Jingyan Han, Masahiro Morita, Amrita Kamat, Nicolas Musi and Mengwei Zang
First published: March 31, 2023, Aging Cell
https://onlinelibrary.wiley.com/doi/10.1111/acel.13811
The University of Texas Health Science Center at San Antonio (UT Health San Antonio) is one of the country’s leading health science universities and is designated as a Hispanic-Serving Institution by the U.S. Department of Education. With missions of teaching, research, patient care and community engagement, its schools of medicine, nursing, dentistry, health professions, graduate biomedical sciences and public health have graduated more than 42,300 alumni who are leading change, advancing their fields and renewing hope for patients and their families throughout South Texas and the world. To learn about the many ways “We make lives better®,” visit UTHealthSA.org.
Stay connected with The University of Texas Health Science Center at San Antonio on Facebook, Twitter, LinkedIn, Instagram and YouTube.
The Sam and Ann Barshop Institute for Longevity and Aging Studies is one of the world’s premier institutes dedicated to the study of age-related diseases. The Barshop Institute is the only aging-intensive research institute in the country to have four peer-reviewed designations: two National Institute on Aging (NIA)-funded centers (Nathan Shock and Claude D. Pepper centers), a testing site of the NIA-sponsored Interventions Testing Program, and a U.S. Department of Veterans Affairs Geriatric Research, Education and Clinical Center.