UT Health San Antonio researchers compared results in less-severe and severe COVID-19 cases one and five months after symptom onset.
Media contacts: Will Sansom, UT Health San Antonio, (210) 567-2579, Sansom@uthscsa.edu
Elizabeth Allen, University Health, (210) 358-2344, Elizabeth.Allen@uhs-sa.com
SAN ANTONIO (Dec. 23, 2021) — Infection-fighting B cells retain better memory of the coronavirus spike protein in University Hospital patients who recover from less-severe cases of COVID-19 than in those recovering from severe COVID-19, a new study suggests. Findings by scientists from The University of Texas Health Science Center at San Antonio were published Dec. 22 in the journal PLOS ONE.

Evelien Bunnik, PhD, corresponding author of the paper, said the results hint of subtle differences in the quality of immune response based on COVID-19 severity. Dr. Bunnik is an assistant professor of microbiology, immunology and molecular genetics at the health science center, also referred to as UT Health San Antonio.
The study focused on memory B cells that react against the SARS-CoV-2 spike protein. Blood samples were analyzed one month after symptom onset and five months post-onset. After one month, a significant proportion of spike-specific B cells were active.
However, samples from eight individuals who recovered from less-severe disease showed increased expression of markers associated with durable B cell memory as compared to individuals who recovered from severe disease, the authors wrote. The markers include T-bet and FcRL5.
T-bet-positive, spike-specific B cells nearly disappeared from the blood samples five months post-symptom onset, the authors noted. Overall, a more dysfunctional B cell response is seen in severe disease cases, they wrote.
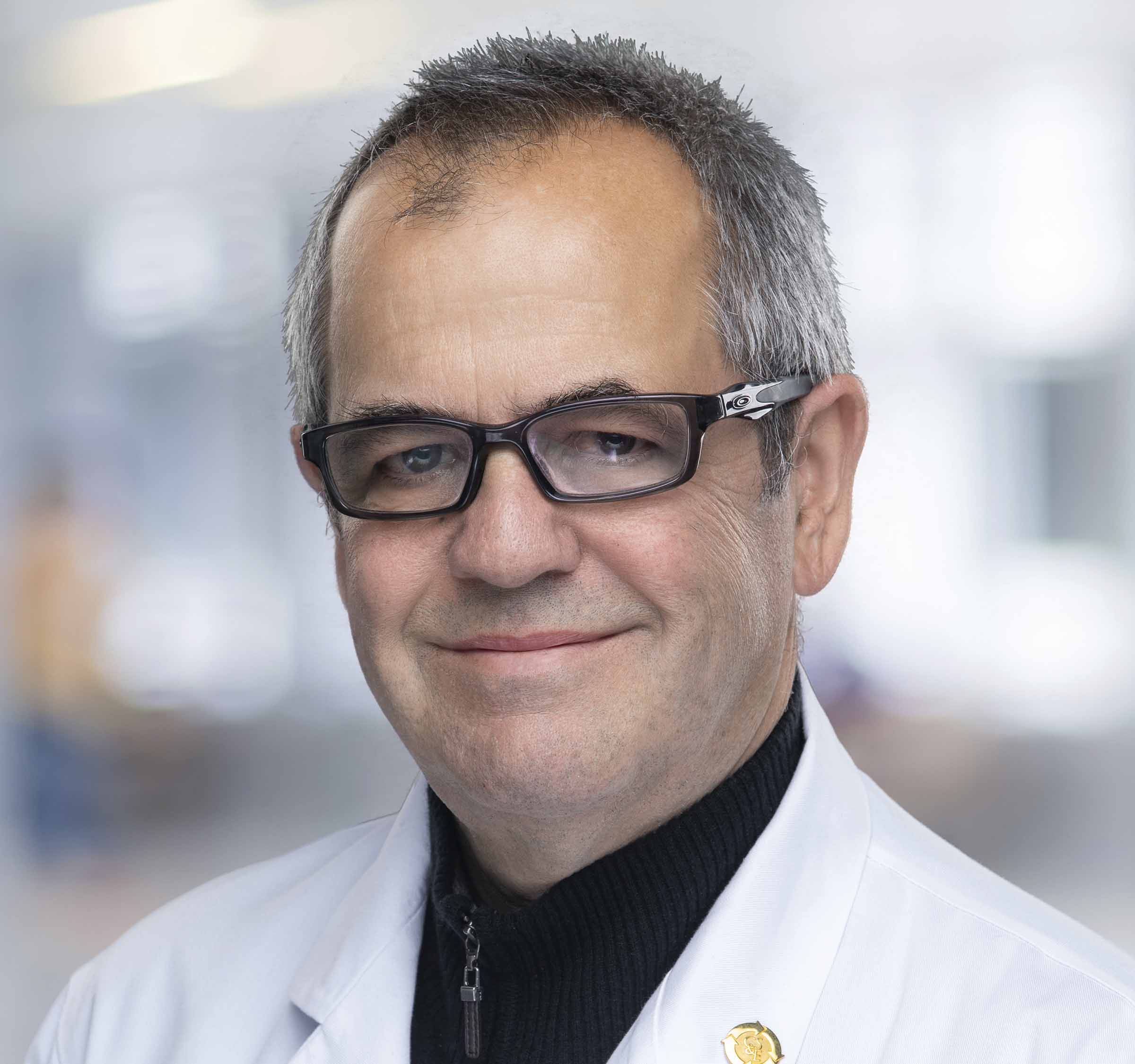
Non-severe cases were defined as not requiring supplemental oxygen or invasive ventilation, while severe cases needed invasive mechanical ventilation or extracorporeal membrane oxygenation (ECMO). “The definition of severe disease was made based on the need for mechanical ventilation or ECMO, because this distinguishes the most critical patients, who are the most likely to develop impaired immune responses,” said study senior author Thomas Patterson, MD, professor and chief of infectious diseases at UT Health San Antonio who leads COVID-19 care at clinical partner University Health.
Study participants were enrolled in the Adaptive COVID-19 Treatment Trial (ACTT)-1 or ACTT-2 clinical trials. Samples were from University Health patients co-enrolled in the UT Health San Antonio COVID-19 Repository.
“The increased percentage of B cells associated with long-lived immunity in non-severe COVID-19 patients may have consequences for long-term immunity against SARS-CoV-2 re-infection or severity of the resulting disease,” the authors wrote.
Acknowledgments
This work was supported by a COVID-19 pilot award from the UT Health San Antonio Joe R. and Teresa Lozano Long School of Medicine (10009547 to Dr. Evelien Bunnik). Raphael A. Reyes was supported by Translational Science Training award TL1 TR002647. Data were generated in the Flow Cytometry Shared Resource Facility, which is supported by UT Health San Antonio, NIH-NCI P30 CA054174-20 (Mays Cancer Center, home to UT Health San Antonio MD Anderson) and UL1 TR001120 (Clinical and Translational Science Award grant). The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
SARS-CoV-2 spike-specific memory B cells express higher levels of T-bet and FcRL5 after non-severe COVID-19 as compared to severe disease
Raphael A. Reyes, Kathleen Clarke, S. Jake Gonzales, Angelene M. Cantwell, Rolando Garza, Gabriel Catano, Robin E. Tragus, Thomas F. Patterson, Sebastiaan Bol and Evelien M. Bunnik
First published: Dec. 22, 2021, PLOS One
https://doi.org/10.1371/journal.pone.0261656
The University of Texas Health Science Center at San Antonio, also referred to as UT Health San Antonio, is one of the country’s leading health sciences universities and is designated as a Hispanic-Serving Institution by the U.S. Department of Education. With missions of teaching, research, patient care and community engagement, its schools of medicine, nursing, dentistry, health professions and graduate biomedical sciences have graduated 39,700 alumni who are leading change, advancing their fields, and renewing hope for patients and their families throughout South Texas and the world. To learn about the many ways “We make lives better®,” visit www.uthscsa.edu.
Stay connected with The University of Texas Health Science Center at San Antonio on Facebook, Twitter, LinkedIn, Instagram and YouTube.
About University Health
University Health is San Antonio’s only locally owned health system and the only academic medical center in South Texas. Its University Hospital serves as the region’s Level I trauma center for adults and children, and is the only area hospital to be state-designated at the highest level for both its Maternity Center and Neonatal Intensive Care Unit. Outpatient care is provided through a comprehensive network of urgent, primary and specialty care centers. For more than 100 years, University Health has been committed to delivering compassionate, culturally competent and high-quality health care, based on a strong foundation of outcomes‐based research and innovative teaching. Learn more at UniversityHealthSystem.com. Follow us on Twitter and Facebook.