By Joe Feist
When UT Health San Antonio’s Robert A. De Lorenzo, MD, was an Army doctor in the bloody Iraq war, he was disturbed by a gap in care due to antiquated airway devices.
“I saw our combat medics and emergency providers not carrying suction equipment, not carrying the best airway equipment,” said Dr. De Lorenzo, professor and research director in the Department of Emergency Medicine. “I asked why, and they said, look, the stuff doesn’t work that great. It’s not worth stuffing into my already overstuffed, too heavy, pack…. We had casualties who were not getting any modern technology” as far as airway management.
Today, as he labors in the emergency department at University Hospital treating COVID-19 patients, including intubating them, he again sees the critical need to advance airway management.
“When a patient’s in respiratory failure, as many COVID patients are, without treatment the patient dies,” said Dr. De Lorenzo. Intubation, or inserting a tube into the trachea, is not easy to do in the best of circumstances, and with COVID-19 there’s a risk of spreading the virus.
Dr. De Lorenzo, also an adjoint faculty member in the Joint Graduate Program in Biomedical Engineering offered by UT Health San Antonio and The University of Texas at San Antonio, is leading a team of researchers in developing a breathing tube suited for 2020, not 1920. His colleagues at UTSA include mechanical engineers.
“Go to medical museums and look at hundred-year-old breathing tubes,” Dr. De Lorenzo said. “They are virtually identical to what we use today. The only difference is back then they were made of dark rubber, today they’re made of clear plastic. In a hundred years we’ve had zero technological advances.”
He said the clear plastic tube used in intubation has one good quality — it’s very inexpensive.
“It has nothing else going for it,” Dr. De Lorenzo said. “It’s hard to place, it’s too stiff, it isn’t flexible, it falls out of place. It doesn’t make a good seal, so you have air leaks. More importantly, fluid from the mouth goes down into the lungs. And if you leave it in too long it causes damage to the airway passage.”
And during the coronavirus pandemic, the leakage of air and fluid poses a definite risk to health care providers.
High-tech materials and modern design such as he and the team are developing can overcome these flaws, Dr. De Lorenzo said. One key is “memory materials” that you bend to a certain shape until you apply a trigger and it changes shape. The resulting endotracheal tube would be easier to insert, expand to stay in place and contract for removal. It would be more secure, thereby limiting the exposure of providers to infection. The new tube would also eliminate the need for multiple-size intubation tubes as one size fits all.
Of course, intubation can’t occur if the airway is blocked. So Dr. De Lorenzo and team are also working on an improved suction device to clear airways.
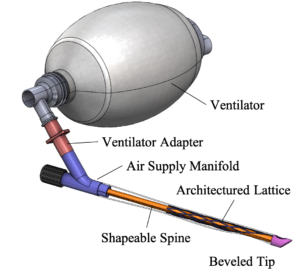 “We’re in the early stages of the venture,” he said. “We’ve developed an early prototype of the breathing tube and we’ve used it on mannequins and we’ve now arranged to use them on cadavers. We’re seeking funding to refine our invention and test it extensively on animals to make sure it’s safe and effective.”
“We’re in the early stages of the venture,” he said. “We’ve developed an early prototype of the breathing tube and we’ve used it on mannequins and we’ve now arranged to use them on cadavers. We’re seeking funding to refine our invention and test it extensively on animals to make sure it’s safe and effective.”
Dr. De Lorenzo said the devices require Food and Drug Administration approval, and he hopes to have a highly refined prototype in 12 to 24 months.
“We are in the airway clearance and securement business,” he said. “We work on inventions that provide paramedics, combat medics, people in the emergency department and even [intensive care units] a better way to clear the airway and secure a modern tube to get it hooked up to a ventilator.”
Whether it’s in a combat field hospital or a modern hospital emergency department, said Dr. De Lorenzo, airway management is definitely an area where innovation is long overdue.
# # #
The Long School of Medicine at The University of Texas Health Science Center at San Antonio is named for Texas philanthropists Joe R. and Teresa Lozano Long. The school is the largest educator of physicians in South Texas, many of whom remain in San Antonio and the region to practice medicine. The school teaches more than 900 students and trains 800 residents each year. As a beacon of multicultural sensitivity, the school annually exceeds the national medical school average of Hispanic students enrolled. The school’s clinical practice is the largest multidisciplinary medical group in South Texas with 850 physicians in more than 100 specialties. The school has a highly productive research enterprise where world leaders in Alzheimer’s disease, diabetes, cancer, aging, heart disease, kidney disease and many other fields are translating molecular discoveries into new therapies. The Long School of Medicine is home to a National Cancer Institute-designated cancer center known for prolific clinical trials and drug development programs, as well as a world-renowned center for aging and related diseases.
The University of Texas Health Science Center at San Antonio, also referred to as UT Health San Antonio, is one of the country’s leading health sciences universities and is designated as a Hispanic-Serving Institution by the U.S. Department of Education. With missions of teaching, research, patient care and community engagement, its schools of medicine, nursing, dentistry, health professions and graduate biomedical sciences have graduated more than 37,000 alumni who are leading change, advancing their fields, and renewing hope for patients and their families throughout South Texas and the world. To learn about the many ways “We make lives better®,” visit www.uthscsa.edu.
Stay connected with UT Health San Antonio on Facebook, Twitter, LinkedIn, Instagram and YouTube.


