The COVID-19 pandemic has interrupted delivery of key health services for children and adolescents, including HPV vaccination for cancer prevention.
The Mays Cancer Center, home to UT Health San Antonio MD Anderson, has partnered with 71 other National Cancer Institute (NCI)-designated cancer centers and partner organizations to issue a joint statement today urging the nation’s health care systems, physicians, parents and children, and young adults to get the human papillomavirus (HPV) vaccination back on track.
Dramatic drops in annual well visits and immunizations during the COVID-19 pandemic have caused a significant vaccination gap and lag in vital preventive services among U.S. children and adolescents—especially for the HPV vaccine. The pandemic also has exacerbated health disparities, leaving Black, Indigenous and other people of color; rural families; and sexual minority adolescents at even greater risk for missed doses of this cancer prevention vaccine.
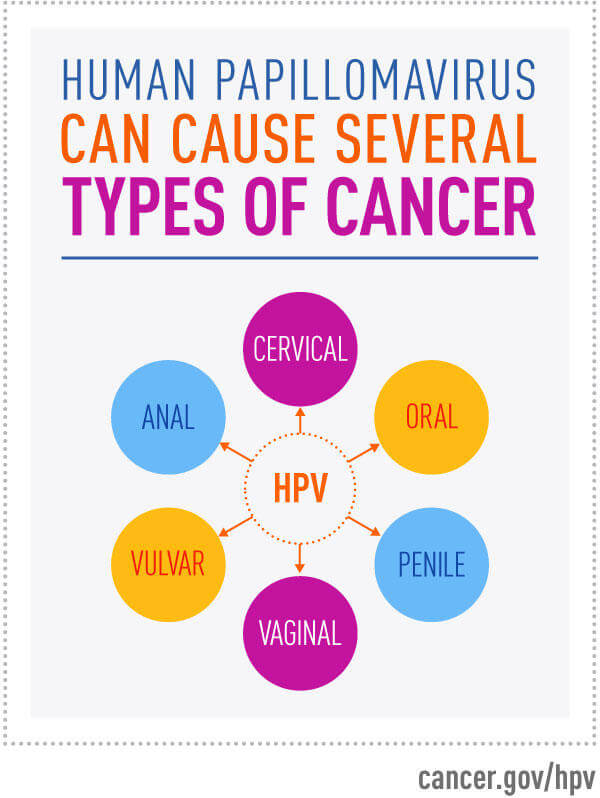
Nearly 80 million Americans – 1 out of every 4 people – are infected with HPV, a virus that causes six types of cancers. Of those millions, nearly 36,000 will be diagnosed with an HPV-related cancer this year. Despite those staggering figures and the availability of a vaccine to prevent HPV infections, HPV vaccination rates remain significantly lower than other recommended adolescent vaccines in the U.S. Even before the COVID-19 pandemic, HPV vaccination rates lagged far behind other routinely recommended vaccines in the U.S. According to 2019 data from the Centers for Disease Control and Prevention (CDC), just more than half (54%) of adolescents were up to date on the HPV vaccine.
Those numbers have declined dangerously since the pandemic:
- Early in the pandemic, HPV vaccination rates among adolescents fell by 75%, resulting in a large cohort of unvaccinated children.
- Since March 2020, an estimated one million doses of HPV vaccine have been missed by adolescents with public insurance— a decline of 21% over pre-pandemic levels.
- Adolescents with private insurance may be missing hundreds of thousands of doses of HPV vaccine.
“This truly is a vaccine that can prevent cancer. It is essential that we vaccinate our children against HPV and that we not let the pandemic change our resolve in doing so,” said Ruben Mesa, MD, FACP, executive director of the Mays Cancer Center.
“Between HPV vaccination and regular gynecologic Pap smear screening, almost all cases of cervical cancer can be prevented,” said Georgia McCann, MD, Mays Cancer Center gynecologic oncology specialist. Dr. McCann is associate clinical professor of obstetrics and gynecology in the Joe R. and Teresa Lozano Long School of Medicine at UT Health San Antonio.
The U.S. has recommended routine HPV vaccination for females since 2006, and for males since 2011. Current recommendations are for routine vaccination at ages 11 or 12 or starting at age 9. Catch-up HPV vaccination is recommended through age 26. Adults aged 27 through 45 should talk with their health care providers about HPV vaccination because some people who have not been vaccinated might benefit. The HPV vaccine series is two doses for children who get the first dose at ages 9 through 14 and three doses for those who get the first dose at ages 15 and older and for immunocompromised people.
NCI Cancer Centers strongly encourage parents to vaccinate their adolescents as soon as possible. The CDC recently authorized COVID-19 vaccination for 12- to 15-year-old children allowing for missed doses of routinely recommended vaccines, including HPV, to be administered at the same time. NCI Cancer Centers strongly urge action by health care systems and health care providers to identify and contact adolescents due for vaccinations and to use every opportunity to encourage and complete vaccination.
“Parents, if you can have your child vaccinated at age 11 or 12 or as early as age 9, that’s really when the HPV vaccine is the most effective, but if your child is older than that, still do not hesitate,” Dr. McCann said.
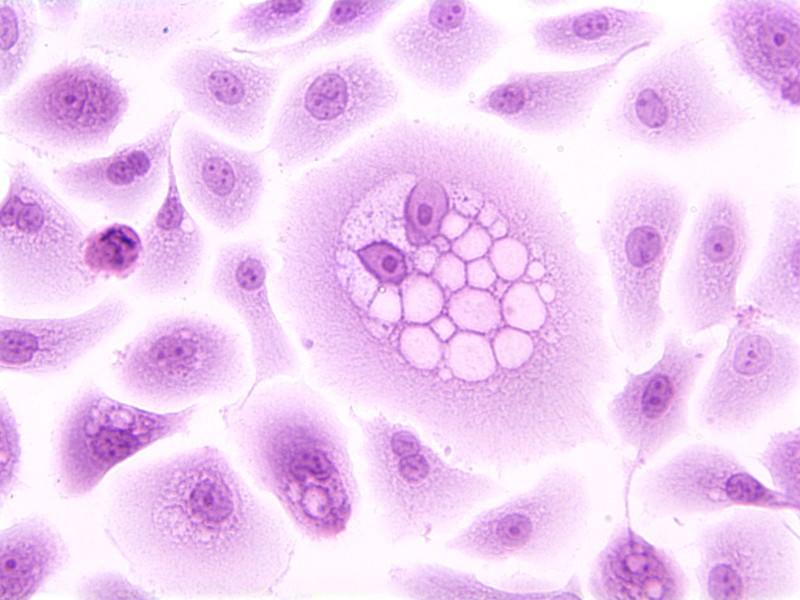
Many people are unaware that they are infected with HPV. The immune system usually clears the virus, just like it does the common cold. But in a small subset of patients, HPV isn’t cleared and the infection can become cancer.
“HPV is controversial because it is sexually transmitted, but the more we talk about it, the more parents we can persuade to vaccinate their young boys and girls and therefore prevent them from getting cancer later in life,” Dr. McCann said.
More information on HPV is available from the CDC and National HPV Vaccination Roundtable. This is the fourth time that all NCI-designated cancer centers have come together to issue a national call to action. All 71 cancer centers unanimously share the goal of sending a powerful message to health care systems, physicians, parents and children, and young adults about the importance of HPV vaccination for the elimination of HPV-related cancers. Organizations endorsing this statement include the Association of American Cancer Institutes; American Association for Cancer Research; American Cancer Society; American Society of Clinical Oncology; American Society of Pediatric Hematology/Oncology; American Society of Preventive Oncology; and Prevent Cancer Foundation.