By Joel Williams
Recognizing and addressing the widespread problem of sleep disorders in military personnel and veterans, the U.S. Departments of Veterans Affairs and Defense (VA/DoD) jointly have issued new guidelines for assessment and treatment of insomnia and obstructive sleep apnea.
“This is a major step for these two organizations in recognizing the importance of appropriately diagnosing and treating sleep disorders in these unique populations,” said Vincent Mysliwiec, M.D., a sleep medicine physician, researcher and retired U.S. Army colonel who helped author the guidelines.
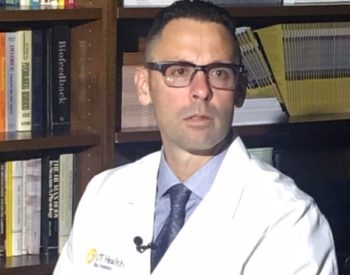
Dr. Mysliwiec, a professor of research in the Department of Psychiatry and Behavioral Sciences at UT Health San Antonio, is also lead author of a synopsis of the guidelines written for the March 2020 issue of Annals of Internal Medicine, a leading medical journal.
Military service is an established risk factor for sleep disorders, which are considerably more prevalent in military personnel and veterans than in the general U.S. population. These populations also have high rates of traumatic brain injury, posttraumatic stress disorder (PTSD), and other mental health disorders, which combined with insomnia and/or sleep apnea complicate treatment of affected military personnel and veterans.
Nearly half of U.S. military personnel have reported poor sleep quality, including insomnia symptoms. Insomnia is one of the most common sleep disorders and affects up to 41 percent of active-duty military personnel deployed to combat zones, 25 percent of noncombatants and 20 percent of those preparing for deployment.
One study found a six-fold increase in sleep disorders among veterans between 2003 and 2010, when millions were deployed to Iraq andAfghanistan. In that study, 4.5 percent of veterans were diagnosed with sleep-disordered breathing, including sleep apnea, a condition in which blockage of the airway interferes with breathing at night. Importantly, sleep apnea increases the risk of cardiovascular disease and motor vehicle crashes. The study also found that 2.5 percent of veterans were diagnosed with insomnia.
Dr. Mysliwiec’s group concluded in the journal article that the actual prevalence of chronic insomnia among veterans likely is considerably higher, because it often is not documented in the medical record. Insomnia can cause daytime sleepiness and cognitive impairment and can adversely affect mental and physical health.
In other research, veterans have reported insomnia rates as high as 50 percent.
The “VA/DoD Clinical Practice Guideline for the Management of Chronic Insomnia Disorder and Obstructive Sleep Apnea” is based on evidence-based and effective therapies for military personnel and veterans with chronic insomnia disorder and sleep apnea, while including evidence from civilian studies. The VA/DoD work group’s 41 recommendations in the clinical practice guideline (CPG) are relevant to all military, VA, and civilian providers who treat patients with sleep disorders.
For treatment of sleep apnea, notable recommendations in the CPG include:
- Use of positive airway pressure therapy (commonly known as CPAP) for the entirety of a patient’s sleep period.
- Continued use of CPAP even with patients who do not use it for at least the common insurance provider standard of four hours per night, while addressing barriers to CPAP adherence.
- Interventions to improve CPAP adherence in patients with sleep apnea and co-occurring PTSD, anxiety, and/or insomnia upon initial diagnosis because these patients have higher rates of non-adherence.
For chronic insomnia, notable recommendations include:
- Cognitive behavioral therapy for insomnia is the recommended treatment, but a shortened version called brief behavioral therapy for insomnia is also acceptable for some patients.
- Sleep hygiene – habits that promote nighttime sleep quality, such as limiting length of daytime naps and avoiding stimulants close to bedtime – while important, should not be used as a stand-alone therapy for chronic insomnia disorder.
- Some medications may be used as a second-line treatment for chronic insomnia, but anti-psychotic drugs and over-the-counter agents such as antihistamine and melatonin are not helpful for treating chronic insomnia.
“We expect the guidelines to be far-reaching and lead to necessary changes in clinical practice while helping to determine what clinical and research questions will need to be addressed in military personnel and veterans,” Dr. Mysliwiec said. “Whereas in the past, problems with sleep disorders have been discounted, there is growing recognition of the importance of sleep health and treating sleep disorders.”
The full VA/DoD clinical practice guideline is available here.
# # #
The Long School of Medicine at The University of Texas Health Science Center at San Antonio is named for Texas philanthropists Joe R. and Teresa Lozano Long. The school is the largest educator of physicians in South Texas, many of whom remain in San Antonio and the region to practice medicine. The school teaches more than 900 students and trains 800 residents each year. As a beacon of multicultural sensitivity, the school annually exceeds the national medical school average of Hispanic students enrolled. The school’s clinical practice is the largest multidisciplinary medical group in South Texas with 850 physicians in more than 100 specialties. The school has a highly productive research enterprise where world leaders in Alzheimer’s disease, diabetes, cancer, aging, heart disease, kidney disease and many other fields are translating molecular discoveries into new therapies. The Long School of Medicine is home to a National Cancer Institute-designated cancer center known for prolific clinical trials and drug development programs, as well as a world-renowned center for aging and related diseases.
The University of Texas Health Science Center at San Antonio, dba UT Health San Antonio, is one of the country’s leading health sciences universities and is designated as a Hispanic-Serving Institution by the U.S. Department of Education. With missions of teaching, research, patient care and community engagement, its schools of medicine, nursing, dentistry, health professions and graduate biomedical sciences have graduated more than 37,000 alumni who are leading change, advancing their fields, and renewing hope for patients and their families throughout South Texas and the world. To learn about the many ways “We make lives better®,” visit http://www.uthscsa.edu.
Stay connected with The University of Texas Health Science Center at San Antonio on Facebook, Twitter, LinkedIn, Instagram and YouTube.


