Ali Seifi, MD, FNCS, FCCM, an associate professor in the Department of Neurosurgery, is quoted in this story in the Smithsonian Magazine.
The Scientist: Special straw may be reliable cure for hiccups
Ali Seifi, MD, FNCS, FCCM, an associate professor in the Department of Neurosurgery, is quoted in this story in The Scientist.
Honors fly high as banners announce School of Medicine’s national ranking

By Kortinae Lozano
In recognition of the U.S. News and World Report’s Best Grad Schools for 2022 rankings, large banners were erected to showcase the Long School of Medicine’s achievement of being named a top 50 medical school for the first time in its history. The banners are located on the facade of the parking garage near the Long School of Medicine on the Long Campus.
In March, the school was named the 16th most diverse medical school in the U.S., a newly added category for U.S. News and World Report.
“Diversity within the medical school means training physicians that are culturally competent and are committed to meeting the unique social and cultural needs of their patients,” said third-year medical student Temiloluwa Adejuyigbe. “As I continue on my journey to become a physician, I am confident that the skills I’ve learned at the Long School of Medicine will equip me to be a supportive physician who seeks to truly understand my patients in the context of their diverse backgrounds.”
The school also received the 46th spot for the best medical school teaching primary care in the United States, as well as 52nd among medical schools performing research. The School of Nursing’s Doctor of Nursing Practice (DNP) degree also was ranked 57th in the 2022 U.S. News & World Report rankings of Graduate Degrees in Nursing.
Dr. Elliot Weser, founding faculty member, passes away at the age of 89
This message from the Dean of the Long School of Medicine was sent on March 27, 2021
The UT Health San Antonio family mourns the passing of Dr. Elliot Weser, a founding faculty member and original Chief of the Division of Gastroenterology and Nutrition, at the age of 89.
Dr. Weser grew up in the Bronx and earned his medical degree at Columbia University College of Physicians and Surgeons, followed by a medical internship at the University of Washington/Harborview Hospital in Seattle and residency at Albert Einstein College of Medicine in New York City. He was accepted into Gastroenterology fellowship at the New York Hospital of Cornell Medical Center, training years that were interrupted 1961‐63 by military service, which he carried out in the U.S. Public Health Service at the National Institutes of Health. After the fellowship, he was recruited to be the third GI faculty member at Cornell under the mentorship of the influential GI pioneer Marvin Sleisenger, but within a few years, he soon felt ready for new challenges.
Approached by Dr. Leon Kander, the founding Chairman of Medicine at what would later become UT Health San Antonio, Elliot joined our faculty in 1967, serving as Chief of Gastroenterology for 11 years and participating in developing the curricula and programs of the new medical school. He was an astute clinician who relished physical diagnosis and sought to build relationships with and support the growing new community of private gastroenterologists in San Antonio, many of whom he trained. His research focused on his passions for small bowel physiology, including carbohydrate metabolism and absorption and short gut syndrome, areas to which he made seminal, novel research contributions.
In 1978, Elliot took on the role of Chief of Medicine at Audie L. Murphy Memorial Veteran’s Administration Hospital, a position that he held for the next 20 years, building a reputation as a shrewd and effective administrator who tirelessly advocated for the clinical, research and teaching missions. Upon his retirement from the VA in 1998, grateful colleagues contributed to the establishment of an endowed Distinguished Lectureship named in his honor, annually bringing world-class speakers to our campus since then as Weser Lecturers.
Throughout his life, Elliot was a passionate supporter of the arts and his synagogue, in particular serving as a co‐founder and leader of Temple Chai. His retirement was enlivened by running successfully for election to the Alamo Heights City Council. Elliot was devoted to his wife, Marcia Goren Weser, and was the proud father both to his son Stephen and to his two step‐daughters, Sara and Leah, through Marcia.
Elliot Weser was a friend, colleague and mentor to countless members of the UT Health San Antonio family. He left an indelible mark on this institution and he will be missed. We are better as an institution because of Dr. Weser’s immense contributions and we are grateful.
Please join me in extending our sincere and heartfelt condolences to Marcia Weser and to the entire family.
Robert Hromas, MD
Dean, Long School of Medicine
Team describes science-based hiccups intervention
Users reported relief in 92% of cases.
Contact: Will Sansom, 210-567-2579, sansom@uthscsa.edu
SAN ANTONIO (June 18, 2021) — Researchers from The University of Texas Health Science Center at San Antonio (UT Health San Antonio) and colleagues worldwide describe a new science-based intervention for hiccups in a research letter published June 18 in the journal JAMA Network Open.
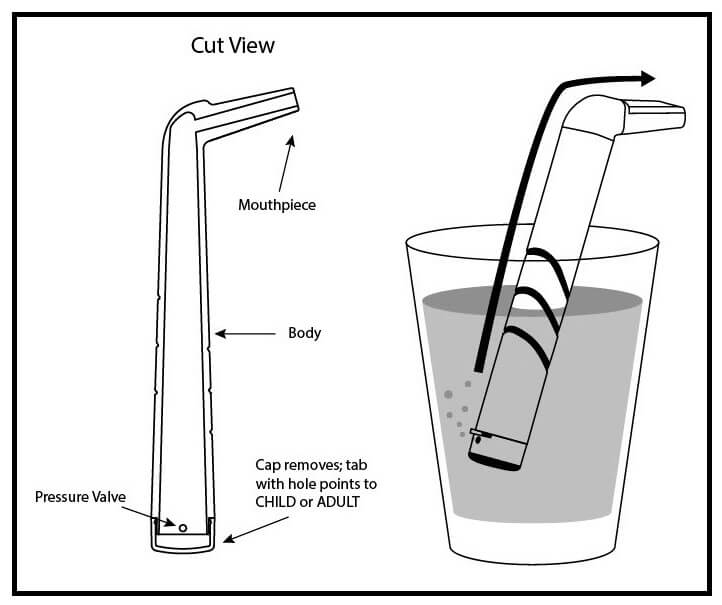
In the publication, the scientists coined a new term for the intervention: the “forced inspiratory suction and swallow tool,” or FISST. The team also reported the results of a survey of 249 users who were asked whether it is superior to hiccup home remedies such as breathing into a paper bag.
The need
“Hiccups are occasionally annoying for some people, but for others they significantly impact quality of life,” said Ali Seifi, MD, associate professor of neurosurgery in UT Health San Antonio’s Joe R. and Teresa Lozano Long School of Medicine. “This includes many patients with brain and stroke injury, and cancer patients. We had a couple of cancer patients in this study. Some chemotherapies cause hiccups.”
Simple tool
FISST is a rigid drinking tube with an inlet valve that requires forceful suction to draw water from a cup into the mouth. The suction and swallow simultaneously stimulate two nerves, the phrenic and vagus nerves, to relieve hiccups.
Forceful suction induces the diaphragm, a sheaf of muscle that inflates the lungs during breathing, to contract. The suction and swallow also prompt the epiglottis, a flap that covers the windpipe during swallowing, to close. This ends the hiccup spasms.
User feedback
FISST stopped hiccups in nearly 92% of cases, users self-reported. In terms of satisfaction, 226 of 249 participants (90.8%) affirmatively answered questions about whether they found the tool easy to use.
On a different measure, subjective effectiveness, 183 of 203 participants (90.1%) indicated that FISST was effective when they used it. Fewer participants answered this question, possibly because it was last in the survey, Dr. Seifi said.
The tool, developed at UT Health San Antonio by Dr. Seifi with input from medical students, is being marketed by a Colorado company under a license agreement with the university and has been accepted by a major supermarket chain to be placed on shelves, Dr. Seifi said.
About the study
The research project began with 600 individuals who, because they stated they had hiccups, received FISST. Of this population, 290 persons responded to a survey about their experience with using the device, compared to other remedies they have used. Of them, 249 fully answered the survey and were included in the research analysis.
The scale was 1 to 5, with 5 meaning the respondents were very happy with FISST and 1 meaning that they preferred to use home remedies.
The respondents were primarily adults over 18 (70%) and were half female and half male. Nearly 80% of the respondents were white.
As far as frequency of hiccups, 69% reported having them at least once a month, and most cases (65%) were transient, less than two hours in duration.
Clinical trial is goal
Future directions include conducting a double-blind clinical trial in Europe and America that gives FISST to one group of trial enrollees and a non-functional, sham device to another group. The challenge is developing something that resembles FISST but doesn’t work, Dr. Seifi said.
Evaluation of the Forced Inspiratory Suction and Swallow Tool to Stop Hiccups
James Alvarez, MD; Jane Margaret Anderson, BSA; Patrick Larry Snyder, MD; Alireza Mirahmadizadeh, MD, MPH, PhD; Daniel Agustin Godoy, MD; Mark Fox, MD, MA; Ali Seifi, MD, FNCS
First published: June 18, 2021, JAMA Network Open
https://jamanetwork.com/journals/jamanetworkopen/fullarticle/2781196
The University of Texas Health Science Center at San Antonio, also referred to as UT Health San Antonio, is one of the country’s leading health sciences universities and is designated as a Hispanic-Serving Institution by the U.S. Department of Education. With missions of teaching, research, patient care and community engagement, its schools of medicine, nursing, dentistry, health professions and graduate biomedical sciences have graduated 39,700 alumni who are leading change, advancing their fields, and renewing hope for patients and their families throughout South Texas and the world. To learn about the many ways “We make lives better®,” visit www.uthscsa.edu.
Stay connected with The University of Texas Health Science Center at San Antonio on Facebook, Twitter, LinkedIn, Instagram and YouTube.
To see how we are battling COVID-19, read inspiring stories on Impact.
LINC Seed Grant awards support pilot projects to foster innovations in interprofessional education

The annual Linking Interprofessional Networks for Collaboration (LINC) Seed Grant Program encourages faculty and staff to develop novel interprofessional education (IPE) activities and promotes IPE research and scholarship.
The program is led by Keith Krolick, PhD, who represents the Graduate School of Biomedical Sciences on the LINC Faculty Council. The council is made up of one faculty representative from each of UT Health San Antonio’s five schools, and teams of faculty and staff they lead, who acquire and disseminate knowledge about IPE.
“After 40 years of teaching, facilitating academic and financial support for so many creative educators is one of the most satisfying things I do these days,” said Dr. Krolick. “The power of interprofessional education will provide our trainees with the collaborative tools and strategies needed to ensure improved health care in the 21st century.”
The 2021 LINC Seed Grant awards will support pilot projects to enhance efforts to provide IPE at UT Health San Antonio.
Selected in May 2021, the newly funded cohort of recipients are listed below, followed by a listing of the previously funded 2019 and 2020 cohorts.
Sadie Velasquez, MD, clinical associate professor in the Long School of Medicine, collaborated with David Ojeda, DDS, clinical assistant professor in the School of Dentistry, on proposals funded in both the 2019 and 2020 cycles.
“With support from LINC, we were able to integrate a longitudinal IPE activity into both the MD and DDS curricula, where students work together in teams over a two-year period,” said Dr. Velasquez. “Importantly, LINC’s support has also helped us present outcomes within Texas and nationally, extending the reach and influence of our work.”
All of the recipients’ efforts contribute to IPE, and also to important institutional goals established for LINC, the Quality Enhancement Plan at UT Health San Antonio.
To date, 31 proposals have been submitted and 18 projects have been funded totaling $80,509. Results of several projects have been presented locally, regionally and nationally.
2021 LINC Seed Grants
A Co-Curricular IPE for Health Professions Students: A World Cafe Approach for Facilitating Knowledge about Interprofessional Collaboration and Patient-Centered Care
Pamela Recto, PhD, RN (PI); Janna Lesser, PhD, RN, FAAN (Co-PI); Andrea Moreno-Vasquez, MPH (Co-PI); Joy Nida Emko, MD, FAAFP (Co-PI); Jose Zapata Jr., MSS (Co-PI)
Health, Equity and the Environment
Adelita Cantu, RN, PhD (PI); Tatjana Walker, MPH, RN, RDN, CDCES, CPH (Co-PI); Roger Perales, MPH (Co-PI); Raymond Palmer, PhD (Co-PI); Sandra Curtis, PhD
Interprofessional Co-Curricular Outreach Program to Promote Healthcare as a Career Opportunity in Underrepresented Minorities in Southwest San Antonio
Darpan Patel, PhD (PI); Irene Chapa, PhD (Co-PI); David Byrd, PhD
Interprofessional Collaboration Including VR and Case Studies for Improved Dementia Care Outcomes
Carol Nguyen, MS (PI); Rebekah Sculley, BSDH, RDH (Co-PI); Carole White, PhD, RN, FAAN (Co-PI); Laura Novak, OTD, OTR, BCG (Co-PI); Jennifer Brackett, MS (Co-PI)
Interprofessional Training with Family Nurse Practitioner (FNP) and Physician Assistant (PA) Students Using Interprofessional Education (IPE) Objective Structured Clinical Examinations (OSCEs)
Sarah Knoeckel, DNP, FNP, MSN, RN (PI); Paula Christianson-Silva, DNP, APRN, FNP-BC, ANP-BC (Co-PI); Steven Skaggs, MPAS (Co-PI); Leticia Bland, DHSc, MPAS, PA-S (Co-PI)
Shades of Success
Irene Chapa, PhD (PI); Sekinat McCormick, MD (Co-PI)
2020 LINC Seed Grants
Clinical Interprofessional Education with Dental and Pharmacy Students to Optimize Pain Management Prescribing in a Dental Surgical Setting
Rebecca Moote, PharmD (PI); Tam Van, DDS (Co-PI); Justina Lipscomb, PharmD (Co-PI); Kirk Evoy, PharmD (Co-PI)
Developing an Interprofessional Objective Structured Clinical Exam (OSCE) for Health Literacy
Melanie Stone, MPH, MEd (PI); Kristy Kosub, MD (Co-PI); Bridgett Piernik-Yoder, PhD, OTR; Rebekah Sculley, RDH; Oralia Bazaldua, PharmD
Interprofessional Education to Enhance the Integration of Oral Health and Medicine: A Longitudinal Study
Sadie Trammell Velasquez, MD (PI); David Ojeda Diaz, DDS (Co-PI); Arthur Don Shaw, DDS; Diane Ferguson, BSN, RN; Cristina Grijalva, MD; Deborah Chang, PhD; Jeff Jackson, EdD
Improving Patient Outcomes through Interprofessional Vascular Sonography Training
Rekha Kar, PhD (PI); Alan Sakaguchi, PhD (Co-PI); Craig Sisson, MD; Omid Rahimi, PhD; Roland Paquette, PA-C; Kimatha Oxford Grice, OTD, OTR, CHT; Ameet Nagpal, MD
Interprofessional Training with Advanced Practice Nurse, Dietetic, and Pharmacy Students Using Nutrition-Focused Case Studies
Wendy Lee, DNP (PI); Christiane Meireles, PhD (Co-PI); Paula Christianson-Silva, DNP (Co-PI); Kirk Evoy, PharmD (Co-PI); Liset Leal-Vasquez, PhD (Co-PI)
2019 LINC Seed Grants
Ergonomics and Musculoskeletal Disorder Interprofessional Education
Juanita Lozano-Pineda, DDS, MPH (PI); Kimatha Oxford Grice, OTD, OTR, CHT (Co-PI); Ricky Joseph, PhD, OTR (Co-PI); Michael Geelhoed, DPT, OCS, MTC (Co-PI)
Head, Ears, Nose, Oral, and Throat Physical Exam Interprofessional Education
Sadie Trammell Velasquez, MD (PI); David Ojeda Diaz, DDS (Co-PI); Diane Ferguson, BSN, RN; Cristina Grijalva, MD; Michaell Huber, DDS; Arthur Don Shaw, DDS
Promoting Interprofessional Collaborative Education (PrICE) for Veterans
M. Danet Lapiz Bluhm, PhD, RN, MSCI (PI); Leticia Bland, DHsc, MPAS, PA-C; Byron Hepburn, MD; Alan Peterson, PhD, ABPP; Robert M. Taft, DDS
Transformative Interprofessional Education: Implementing a Workshop on Interprofessional Collaboration and Communication
Jason Morrow, MD, PhD, FAAHPM (PI); Carlos Herrera, BS, MOT student
Trifecta: When Social Determinants of Health, Interprofessional Education and a School Based Prevention Program Meet
Adelita Cantu, PhD, RN (PI); Rebekah Salt, PhD, RN (Co-PI); Georgiana Gross, MPH, RD/LD (Co-PI)
VAPE: Vaping Assessment, Prevention and Education Project
Tammy Harris, DMSc, MPAS, PA-C (PI); Leticia Bland, DHsc, MPAS, PA-C; Ryan Van Ramshorst, MD, FACP; Roland Paquette, MPAS, PA-C; Meredith Quinene, DSc, MPAS, PA-C; Thomas Stokes, Jr., MEd, RTT; Sandeep Subramanian, BPTh, PhD
We Care: Learning Together to Support Family Caregivers
Carole White, PhD, RN, FAAN (PI); Jennifer Brackett, MSG; Cindy Sikora, DNP, RN; Bridgett Piernik-Yoder, PhD, OTR; Precious Osuoha, PhD, OTR; Fang-Ling Lu, PhD, CCC-SLP; Rocio Norman, PhD, CCC-SLP
To learn more about LINC, click here.
Learn more about the LINC Seed Grant Program.
Read LINC advances interprofessional education to train health care leaders.

