Kristin Ann Altwegg, a fourth-year student in the Graduate School of Biomedical Sciences at UT Health San Antonio, was selected to participate in the AACR Early Career Hill Day on Feb. 25. Altwegg is an affiliate member of the Mays Cancer Center, home to UT Health San Antonio MD Anderson, and is in the Cancer Biology discipline of the graduate school’s Integrated Biomedical Sciences Program.
The event, offered by the American Association for Cancer Research (AACR), was held virtually this year due to the COVID-19 pandemic. Altwegg and 21 other early career cancer scientists from across the United States met with nearly 60 members of Congress and their staff, representing 17 different states.
Early Career Hill Day is an opportunity for graduate students, postdoctoral fellows and other early career cancer scientists to meet with members of Congress and/or their staff to convey the importance of robust, sustained and predictable federal funding for medical research.
Altwegg’s biosketch for AACR Early Career Hill Day noted that she “is committed to improving our understanding of breast and gynecologic cancers with a goal of developing next-generation translational cancer therapeutics and prevention interventions to positively enhance disease-free interval and survival outcomes.”
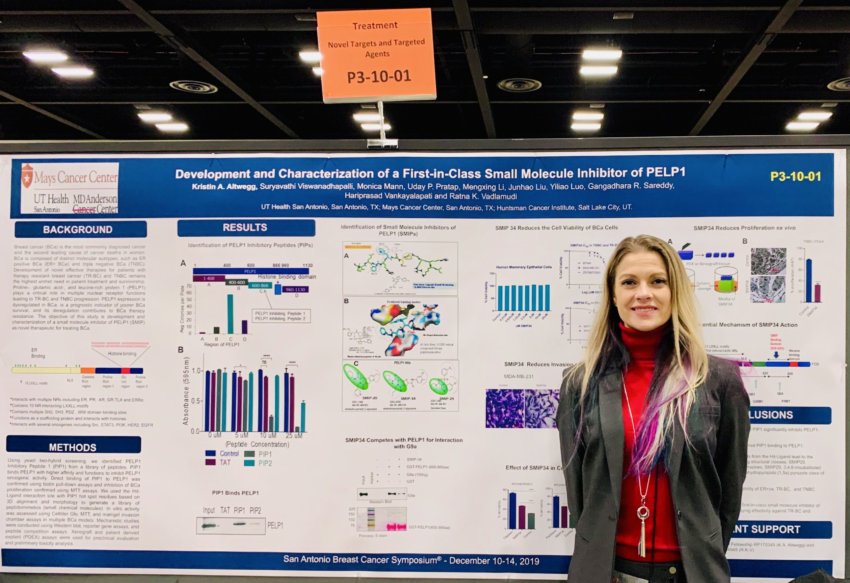
Altwegg, a CPRIT Predoctoral Fellow, received an AACR Associate Member Award for her poster at the San Antonio Breast Cancer Symposium (SABCS) in December 2019. Read a story about her SABCS experience here.
CPRIT is short for Cancer Prevention and Research Institute of Texas.
Her research is dedicated to uncovering the mechanistic contributions of oncogenes, epigenetics and hormonal signaling, with an eye toward the development of novel translational advances in women’s cancer therapeutics, the biosketch continues.
Congratulations to Kristin Altwegg.