Ruben A. Mesa, M.D., director of Mays Cancer Center at the newly named UT Health San Antonio MD Anderson Cancer Center, discusses the approval of fedratinib (Inrebic) in myelofibrosis and other JAK inhibitors in the treatment pipeline.
Targeted Oncology: Highlighting current advances for the treatment of myeloproliferative neoplasms
Ruben Mesa, M.D., director of the Mays Cancer Center, home to UT Health San Antonio MD Anderson Cancer Center, discusses the current state of the treatment landscape for patients with myeloproliferative neoplasms (MPNs).
Liver cancer prevention project boosts hepatitis C screening and care in safety-net practices
Medications today can cure hepatitis C virus infection in only a few months and prevent liver cancer and severe liver damage from chronic infection. However, most patients in safety-net primary care practices are not being screened for the virus—even those most at risk.
“It is estimated that 1.5 million people in the U.S. have chronic HCV infection and don’t know it. It’s a huge public health issue,” said Raudel Bobadilla of the university’s Center for Research to Advance Community Health (ReACH) Center. South Texas is disproportionately affected by liver cancer.
Small practices that manage uninsured patients lack the infrastructure necessary to accomplish widespread HCV screening, a team of researchers from the Long School of Medicine discovered. Nationally, screening rates are less than 20%.
The researchers tested a screening intervention program at five federally qualified health centers and one family medicine residency program that serve low-income communities with largely Hispanic populations. The program is supported by a grant from the Cancer Prevention and Research Institute of Texas (CPRIT) and the Centers for Medicare and Medicaid Services.
“Our program…aims to arrest the rise in Texas liver cancer by building the capacity of primary care settings to screen for HCV infection as well as to manage and treat infected patients within their medical home through teleconsultation,” said study co-author Andrea Rochat of the Long School of Medicine. Rochat is a senior research coordinator with the ReACH Center.
The program, called Screen, Treat or Prevent Hepatocellular Carcinoma and Hepatitis C Virus (STOP HCC-HCV), increased screening rates at the six health centers in baby boomers—the post-World War II generation most at risk—from less than 1% to 48%. Results were published in December in the journal Annals of Internal Medicine.
“In the practices we studied, HCV screening of baby boomers was not happening at baseline,” said study senior author Barbara J. Turner, M.D., who led the study at the Long School of Medicine and is transitioning to the University of Southern California’s Keck School of Medicine.
The program also supported teleconsultation specialist support and training so that primary care physicians could treat uninsured patients with chronic HCV infection who cannot access specialist care but are able to receive HCV medications through programs for low-income patients. Ninety-five percent of the uninsured patients who started treatment during the program were cured.
HCV infection is underdiagnosed and can persist in a patient for decades before presenting symptoms. The U.S. Preventive Services Task Force in 2013 recommended one-time HCV screening for everyone born in 1945 through 1965. Three-fourths of people infected with HCV are in that age group and were infected years ago due to less-effective sterilization in health care delivery, injection drug use and blood transfusions before HCV screening.
Since 2013, the prevalence of HCV has increased in younger people, and oral direct-acting antiviral medications have been introduced to treat the disease safely and quickly.
The Preventive Services Task Force in August 2019 released a draft recommendation statement seeking public input on expanding one-time screening for HCV infection to all adults ages 18-79.
“Although these guidelines are still considered to be a draft, the field recognizes that these will likely become formal guidelines soon,” said study co-author Sarah Lill of the ReACH Center.
The guideline requires an effective infrastructure within primary care that will allow for screening, treatment and long-term management. The program can be used to create future models for the screening of all adults for the virus, Rochat said.
According to the American Cancer Society, 4,300 Texans were diagnosed with liver cancer in 2019 and 2,800 died of the disease. Worldwide, long-term infection with hepatitis C and hepatitis B virus is the most common risk factor for liver cancer.
“The take-home message is that we have national guidelines to test every baby boomer and may shortly have recommendations to test all adults for HCV, but we need to develop and support the infrastructure to put screening and management into place for vulnerable populations,” Dr. Turner said.
Read more about the program.
A Higher Call: Chris Heins

“I think the care I’ve provided for critically injured soldiers pushed me to want to learn more, so I could do more for them.”
At age 22, Chris Heins dropped out of college. With little drive and no real plan, Heins was looking for a sense of direction, discipline in his life and an opportunity to reset. That opportunity came in 2009, when he enlisted in the United States Army as a Combat Medic Specialist (68W) and found a higher purpose.
 After three years of active duty service, Heins felt the call to do more. He transitioned to the Army Reserve in order to attend the UT Health San Antonio School of Nursing in pursuit of becoming an Emergency Room Nurse (66T).
After three years of active duty service, Heins felt the call to do more. He transitioned to the Army Reserve in order to attend the UT Health San Antonio School of Nursing in pursuit of becoming an Emergency Room Nurse (66T).
After graduating and becoming an emergency nurse, Heins again began to feel the call to do more. “I think the care I’ve provided for critically injured soldiers pushed me to want to learn more, so I could do more for them,” Heins said. That drive alongside the mentorship and confidence of the physicians he worked with while serving is what led him down his admittedly complicated route to medical school.
He credited his prior service with giving him the skills and drive to continue his academic career, saying, “I would certainly not be here now if not for the mental fortitude I learned during my enlisted time. My ability to simply put my head down and grind helped get me to this point and it has been a boon[1] in my schooling so far.”
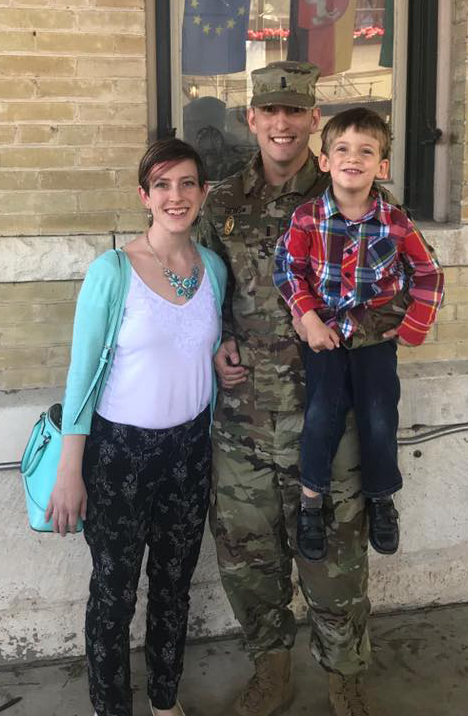
His drive and mental fortitude pushed him to achieve his goal of doing everything he can to care for ill and injured soldiers. “Emergency medicine is the most immediate way for me to provide care closest to the point-of-wounding, during the most critical period of patient care,” he said.
Heins’ daily schedule shows his commitment to his mission. He starts his day at the gym at 4:45 a.m. From there, he arrives home to help his son get ready for school. He reviews the previous day’s class notes over breakfast and is off to attend mandatory lectures until noon. His afternoons consist of more study time and participation in extracurricular groups such as the Emergency Medicine Student Association and the Military Health Interest Group. Even with this hectic schedule, he still picks his son up from school, prepares dinner, and eats with his family every night before prepping for the next day.
While he recognizes that military medicine was the best path for him, it may not be the best for all. “I certainly encourage anyone considering military medicine to talk with someone who previously served,” Heins encouraged. “There are so many small things that never occurred to me prior to serving. San Antonio has a glut[2] of current and former military doctors, the vast majority of whom are willing to talk to students about their experiences. Use this network to find a mentor who can tell you what to expect within your chosen specialty, as it could be totally different from a civilian experience.”
Heins’ story reminds us of what it takes to pursue the higher calling in life – hard work, dedication, and perseverance.
[1] Definition of boon: a timely benefit
[2] Definition of glut: an excessive quantity
Cork tree bark extract, exercise each slow aggressive prostate cancer
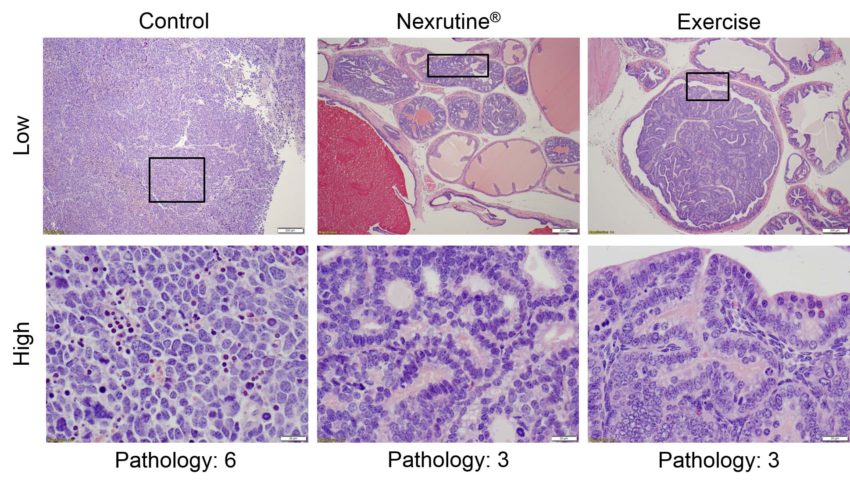
Researchers from UT Health San Antonio are the first to show that a natural supplement made from the bark of cork trees is as effective as exercise in preventing the progression of aggressive prostate cancer.
“Nexrutine is an herbal extract from the bark of the cork tree Phellodendron amurense. It is widely used to treat inflammation, gastroenteritis, abdominal pain and diarrhea,” Dr. Darpan Patel, Ph.D., associate professor of research in the School of Nursing, who led the study said.
In the study, supported by pilot funds from the Mays Cancer Center, home to UT Health San Antonio MD Anderson Cancer Center, 45 mice were divided into three groups.
One group received food pellets supplemented with the cork tree extract, Nexrutine. The second group received free access to a running wheel. The third was the control group, which received no treatment.
The results showed that the group receiving the cork tree extract had 62% less tumor growth, while the exercise group had 60% less tumor growth, compared to the control group.
“It appears that both Nexrutine and exercise work equally well but use different pathways,” Dr. Patel said.
The research team came to this conclusion by evaluating the tumors and levels of various inflammatory markers in the blood after the 20-week study.
They learned that mice in both treatment groups had a lower level of a type of protein that regulates inflammation and the expression of genes involved in the growth and survival of cancer cells, called Interleukin 1 alpha (IL-1a), and the formation of abnormal blood vessels that support tumor growth.
However, they were surprised to learn that the two treatment groups had some differences, indicating different pathways may be involved.
Pratap Kumar, Ph.D., professor in the UT Health San Antonio Department of Molecular Medicine, was a key investigator on the study, published on Dec. 19 in the journal PLOS ONE.
Dr. Kumar has carried out extensive work with Nexrutine in various cancers including a clinical study in prostate cancer patients.
Dr. Patel said that more research will be needed to better understand the separate mechanisms and how they work.
“Perhaps a combination treatment could be developed in the future that would attack the cancer on several fronts,” he said. “Nexrutine also may be a good alternative for people who find it difficult to exercise,” Dr. Kumar said.
Both Drs. Patel and Kumar are members of the Population Sciences and Prevention program of Mays Cancer Center, a National Cancer Institute-designated cancer center. Dr Kumar is also co-leader of this program.
“The results of these research studies by Mays Cancer Center investigators is deeply exciting. If confirmed in subsequent human clinical trials, the discovery of this new way to control aggressive prostate cancer is an important addition to our arsenal against cancer,” said Mays Cancer Center Director Ruben Mesa, M.D., FACP.
According to the American Cancer Society, prostate cancer is the second most common type of cancer in men behind skin cancer and is the second-leading cause of cancer deaths in men after lung cancer.
AJMC: Dr. Ruben Mesa outlines the quality of life impact of myelofibrosis
Ruben Mesa, MD, director of Mays Cancer Center, home to UT Health San Antonio MD Anderson Cancer Center, discusses the impact myelofibrosis has on patients’ quality of life while at the American Society of Hematology conference.
Dr. Mesa describes the symptoms of myelofibrosis and notes that a majority of patients have notable discomfort related to their disease.

