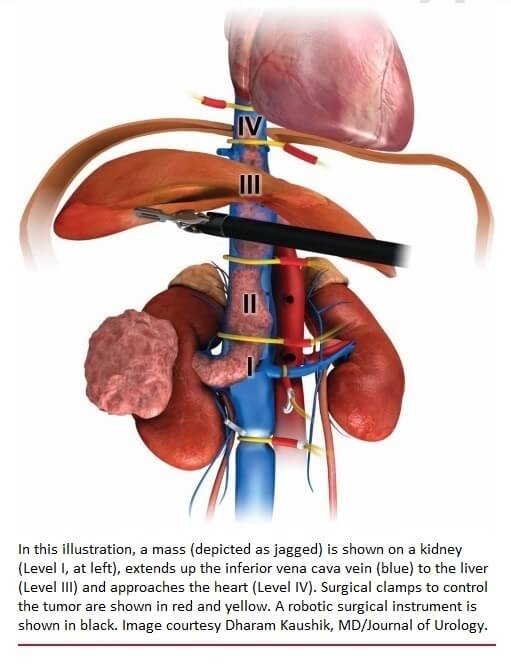
Kidney cancer is not always confined to the kidney. In advanced cases, this cancer invades the body’s biggest vein, the inferior vena cava (IVC), which carries blood out of the kidneys back to the heart. Through this vein, cancer may infiltrate the liver and heart. The Mays Cancer Center at UT Health San Antonio is one of the high-volume centers in the U.S. with surgical expertise in treating this serious problem. The Mays Cancer Center is San Antonio’s National Cancer Institute-designated Cancer Center.
In a study featured on the cover of the Journal of Urology (Official Journal of the American Urological Association), researchers from the Mays Cancer Center and Department of Urology show that robotically removing cancer from the inferior vena cava is a safe and effective alternative to the standard open surgery.
Through IVC thrombectomy, the affected kidney is removed along with the tumor. The surgery is performed at UT Health San Antonio’s clinical partner, University Hospital.
Harshit Garg, MD, urologic oncology fellow in the Department of Urology, is first author of the study, and Dharam Kaushik, MD, urologic oncology fellowship program director, is the senior author. Kaushik is an associate professor and the Stanley and Sandra Rosenberg Endowed Chair in Urologic Research at UT Health San Antonio.
The open surgery requires an incision that begins 2 inches below the ribcage and extends downward on both sides of the ribcage. Surrounding organs must be moved so surgeons can access the inferior vena cava for cancer resection.
“Open surgery has an excellent success rate, and most cases are performed in this manner,” Kaushik said. “But now, with the robotic approach, we can achieve similar results with smaller incisions. Therefore, we need to study the implications of utilizing this newer approach.”
The authors reviewed and analyzed data from 28 studies that enrolled 1,375 patients at different medical centers. Of these patients, 439 had robotic IVC thrombectomy and 936 had open surgery. Kaushik and his team collaborated with Memorial Sloan Kettering Cancer Center, New York; Cedars-Sinai Medical Center, Los Angeles; and the University of Washington, Seattle, to perform this study.
“We pulled the data together to make conclusions because, before this, only small studies from single institutions had been conducted to compare the IVC thrombectomy approaches,” Kaushik said.
 Findings
Findings
The results are encouraging, finding:
- Fewer blood transfusions: 18% of robotic patients required transfusions compared to 64% of open patients.
- Fewer complications: 14.5% of robotic patients experienced complications such as bleeding compared to 36.7% of open thrombectomy patients.
These large, technically challenging surgeries last eight to 10 hours and involve a multidisciplinary team of vascular surgeons, cardiac surgeons, transplant surgeons and urologic oncology surgeons, Kaushik said.
This is the largest study to analyze the outcomes of robotic versus open IVC thrombectomy, Kaushik said.
While open surgery remains the gold standard for surgery, the study shows it could be a good option for certain patients, he said.
“Optimal candidacy for a robotic surgery should be based on a surgeon’s robotic expertise, the extent and burden of the tumor, and the patient’s comorbid conditions,” Kaushik said.
For more detailed information about this study, the full release is available here.


