Rare species documented for the first time in several states, Canada
Growing concern over a potential increase in fungal strains resistant to typical treatments led investigators at The University of Texas Health Science Center at San Antonio to take a closer look at dermatophytes and levels of antifungal-drug resistance.
Dermatophytosis, an infection of the skin, hair or nails caused by a group of fungi called dermatophytes, is the most common fungal infection seen worldwide. While dermatophytosis is generally considered a minor condition, it can lead to great discomfort and cosmetic concerns.
In the United States and Canada, most dermatophyte infections are caused by the species Trichophyton rubrum (T. rubrum) or members of the Trichophyton mentagrophytes complex.
Nathan Wiederhold, PharmD, director of the Fungus Testing Laboratory at UT Health Science Center San Antonio, said his lab conducts regular susceptibility testing of yeasts and molds.
Study of 2021-2022 samples: What they found
“It was about the end of 2021, beginning of 2022, we started to notice some results that were a little strange. We hadn’t seen this before,” he said.
Wiederhold said there was a significant increase in cultures of dermatophytes showing resistance to the antifungal terbinafine. Terbinafine is a common first-line treatment for dermatophytosis.
During this time, Wiederhold said he was contacted by members of the Mycotic Diseases Branch at the Centers for Disease Control and Prevention who also noticed a trend in terbinafine-resistant dermatophytes that had been reported in other countries.
The lab examined strains prospectively and retrospectively from several states and parts of Canada from 2021 through 2022.
During these two years, there were 271 dermatophyte isolates, most of which were susceptible to terbinafine.

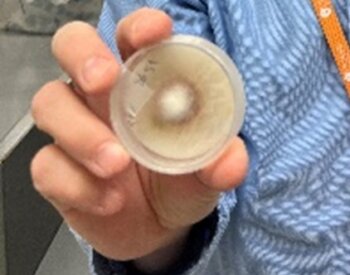
However, nearly 19% of samples showed high resistance to terbinafine (brand name Lamasil). About half of the resistant strains assessed were a novel species called Trichophyton indotineae (T. indotineae), but the other half surprisingly were the more common T. rubrum.
A deeper dive into the historical database in the Fungus Testing Laboratory from 2001 through 2020 showed other cases of resistant dermatophytes in this time as well, along with the discovery of three earlier isolates of T. indotineae, with the earliest strain being received in the lab in 2017.
Over the past decade, T. indotineae has spread widely across India and parts of South Asia, with reports now documenting the species in other countries in Asia and Europe. This is a hyper-virulent species that can lead to severe skin conditions. It can be highly resistant to terbinafine and azole drugs, such as itraconazole, which can also be used to treat dermatophytosis.
The study at the health science center lab showed T. indotineae is now widespread in the U.S. and in some provinces in Canada.
Wiederhold said they knew T. indotineae was making its way around the world and it was only a matter of time before it came to the United States. But what was not expected was the antifungal resistance they observed in the more common cause of dermatophytosis, T. rubrum.
What is causing this resistance?
Wiederhold said a driving force behind antifungal resistance in some parts of the world is the availability of over-the-counter products that contain combinations of antifungals, antibiotics and steroids.
“It’s the availability of these products that contain an antifungal, antibiotic and they also contain steroids and their widespread availability in products that can be obtained without a prescription. Steroids are kind of like throwing gasoline onto a fire when you’re talking about fungal infections,” Wiederhold said.

Topical steroids can dampen the immune response, which allows the fungi to grow unchecked.
Wiederhold said to combat this potential problem, the CDC is promoting education for the public, dermatologists and primary care physicians.
“It’s now in our backyard. Education is going to be a very important thing,” he said.
The CDC and others are also pushing for the availability of new tests that can quickly identify not only the type of fungus present but also if it may be drug resistant.
Similar tests are already available in Europe, Wiederhold said, but such a test in the U.S. is not commercially available at this time.
If a test were developed, the approval process could take time, Wiederhold said, as it would have to go through the regulatory process and clearance by the Food and Drug Administration.
What if that doesn’t work?
Wiederhold said there is a limited number of options for treatment of these types of fungal infections. Here in the U.S. and Canada, if an infection is not responding to terbinafine, the next step would be a treatment from the azole class or other antifungals.
“If you have resistance to those, you’re starting to run out of options,” he said.
Wiederhold said the lab maintains surveillance of samples and, unfortunately, continues to see isolates with resistance.
Wiederhold said this study was the result of “team science” as a collaboration between his lab, the Molecular Diagnostics Laboratory led by associate professor Marjorie David, MD, from the Department of Pathology and Laboratory Medicine and working closely with the CDC.
Wiederhold and his team’s study was published in the August 2023 Journal of Clinical Microbiology. The CDC also wrote a commentary on the study in the December 2023 issue of the journal.
Terbinafine-Resistant Dermatophytes and the Presence of Trichophyton indotineae in North America
Connie F. Cañete-Gibas, James Mele, Hoja P. Patterson, Carmita J. Sanders, Dora Ferrer, Victor Garcia, Hongxin Fan, Marjorie David, Nathan P. Wiederhold
First published: July 11, 2023, Journal of Clinical Microbiology, https://journals.asm.org/doi/10.1128/jcm.00562-23
Commentary from CDC: Trichophyton indotineae and other terbinafine-resistant dermatophytes in North America
Shawn R. Lockhart , Dallas J. Smith, Jeremy A. W. Gold
First published: November 28, 2023, Journal of Clinical Microbiology, https://journals.asm.org/doi/10.1128/jcm.00903-23
The University of Texas Health Science Center at San Antonio (UT Health San Antonio) is one of the country’s leading health science universities and is designated as a Hispanic-Serving Institution by the U.S. Department of Education. With missions of teaching, research, patient care and community engagement, its schools of medicine, nursing, dentistry, health professions, graduate biomedical sciences and public health have graduated more than 42,550 alumni who are leading change, advancing their fields and renewing hope for patients and their families throughout South Texas and the world. To learn about the many ways “We make lives better®,” visit UTHealthSA.org. Stay connected with The University of Texas Health Science at San Antonio on Facebook, Twitter, LinkedIn, Instagram and YouTube.


